In this section we will cover each of the cranial nerves and how they can be examined clinically. We will also cover the associated nuclei:
When you're feeling confident check out our CRANIAL NERVES QUIZ to test your own knowledge!
CRANIAL NERVE I: OLFACTORY NERVE
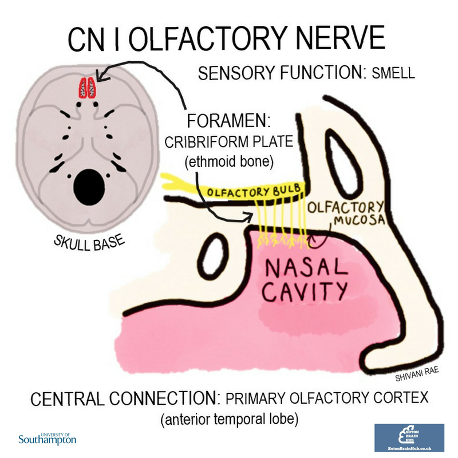
The olfactory nerve has just a special sensory function: the sense of smell. Olfactory receptor cells in the olfactory mucosa pass through holes in the cribriform plate and synapse in the olfactory bulb. The olfactory bulbs continue as the olfactory tracts to the primary olfactory cortex and associated areas.
Remember, the olfactory nerve (along with the optic nerve) differs from the other cranial nerves in that it doesn’t arise from the brainstem.
Check out our video below to find out how to assess the function of CN I:
CRANIAL NERVE II: OPTIC NERVE
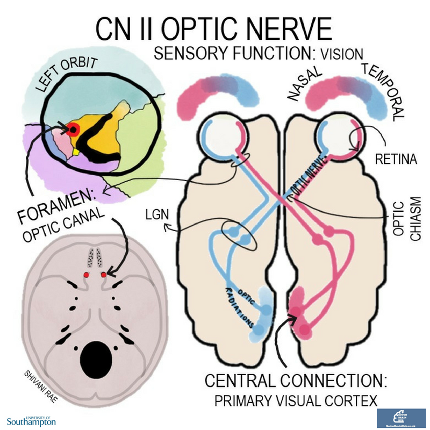
The optic nerves are solely sensory. They convey visual information from each retina out of the eye and into the skull through the optic canals.
The left and right optic nerves meet to form the optic chiasm, where fibres from the nasal half of each retina cross over. The optic tract continues to the lateral geniculate nucleus in the thalamus, from where optic radiations fan out to the primary visual cortex in the occipital lobe.
The visual pathway is a useful diagram to be able to draw as it allows you to figure out where a lesion is when presented with a visual field deficit. Just shade in the parts of the visual field that are lost and track along the pathway to find the lesion! Using this method you can see for yourself how bitemporal hemianopia (bilateral loss of the temporal visual field) is most likely caused by damage at the optic chiasm. Enlargement of which nearby structure may be responsible for compression of the optic chiasm.
Check out our video below to learn how to examine the function of CNII:
CRANIAL NERVE III: OCULOMOTOR NERVE
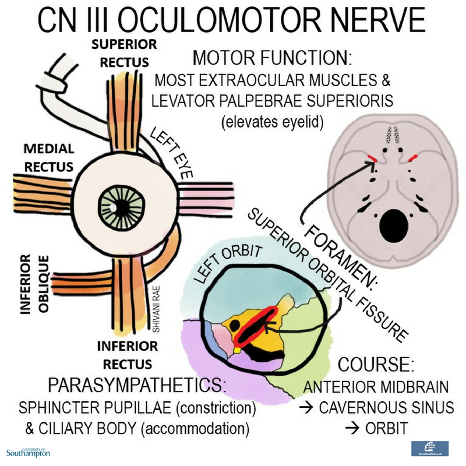
The oculomotor nerve originates in the anterior medulla and passes anteriorly before passing through the cavernous sinus and exiting the skull through the superior orbital fissure.
Its motor function is to supply levator palpebrae superioris (which elevates the upper eyelid) and 4 of the 6 extraocular muscles: superior rectus, inferior rectus, medial rectus and inferior oblique. For a refresher on the actions of each of these muscles check out our post on the MUSCLES OF THE EYE!
The oculomotor nerve also has parasympathetic functions, supplying both the sphincter pupillae (which constricts the pupil) and the ciliary muscles (which mediate accommodation to nearby objects by making the lens more spherical).
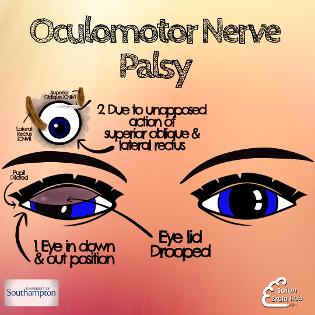
Clinical clue 1: Third nerve palsy
When the oculomotor nerve no longer works properly the position of the eye is a reflection of those muscles that are able to continue to work because they are not innervated by the third nerve. Typically the eye is pulled into a down and out position. The eyelid droops (called ptosis) and the pupil will change size to become larger in comparison to the non affected , because of the continued healthy innervation from the sympathetic nervous system.
Third nerve palsy can be caused by an aneurysm of the posterior communicating artery due to their close anatomical relationship.
Check out our resources below to learn more about third nerve palsy:
CRANIAL NERVE IV: TROCHLEAR NERVE
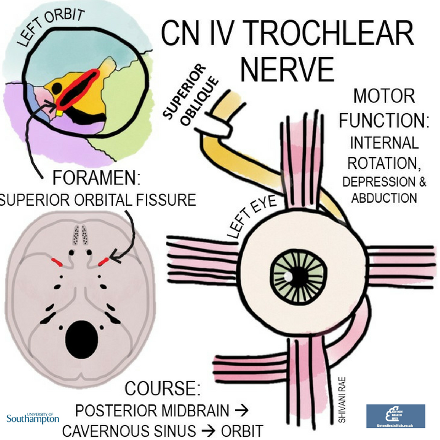
The trochlear nerve emerges from the posterior midbrain and, like the oculomotor nerve, passes through the cavernous sinus and exits the skull through the superior orbital fissure.
It supplies the superior oblique extraocular muscle, the actions of which are a little more complex than the recti. The key is to remember that the superior oblique passes through a pulley-like structure (trochlea is Latin for pulley), making its primary actions to internally rotate and depress the eye.
Clinical clue 2: Trochlear nerve palsy
Damage to the trochlear nerve results in paralysis of the superior oblique muscle. This typically presents with vertical diplopia made worse when looking down (classically when walking down the stairs). People may begin to tilt their head to compensate. Their head will tilt away from the affected side.
Check out our video below to learn more about trochlear nerve palsy:
CRANIAL NERVE V: TRIGEMINAL NERVE
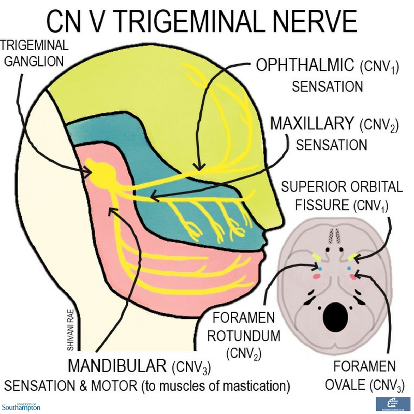
The trigeminal nerve emerges at the level of the pons as a sensory and a motor root. The sensory root branches into three at the trigeminal ganglion, giving rise to the ophthalmic, maxillary and mandibular nerves.
The ophthalmic and maxillary nerves pass through the cavernous sinus and exit the skull through the superior orbital fissure and the foramen rotundum respectively.
The motor root joins up with the mandibular nerve, giving this branch a motor function in addition to its sensory role. The mandibular nerve leaves the skull via the foramen ovale.
The main function of the three branches is sensation to the skin, mucous membranes and air sinuses in the distributions shown in the diagram. The main motor function of the mandibular nerve is supply to the muscles of mastication.
Note that while the trigeminal nerve has no parasympathetic supply of its own, each of the three branches carries parasympathetic fibres from other cranial nerves
Check out our videos below on the trigeminal nerve:
CRANIAL NERVE VI: ABDUCENS NERVE
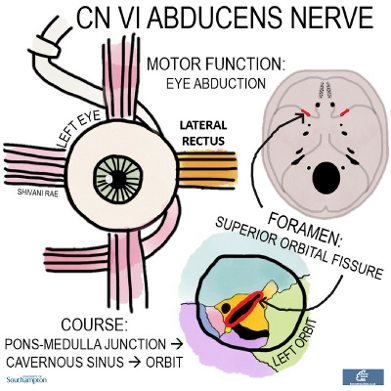
The abducens emerges from the pons-medulla junction and travels anteriorly, through the cavernous sinus and out of the skull through the superior orbital fissure. It innervates just one extraocular muscle - the lateral rectus, which abducts the eyeball
Clinical clue 3: Abducens nerve palsy
Clinically abducens palsy will present with slight adduction of the affected eye due to unopposed tonic action of the medial rectus . The patient will experience binocular horizontal diplopia when looking to side of affected eye.
There are a number of causes of abducens nerve palsy. These include- cavernous sinus thrombosis, cavernous sinus fistula and internal carotid aneurysm. It can also be cause by orbital pathologies such as neoplasm, inflammatory diseases, infection or trauma
Check out our video below to learn more about the abducens nerve:
Check out our video below to learn more about how to examine the function of CN III, CN IV and CN VI:
CRANIAL NERVE VII: FACIAL NERVE
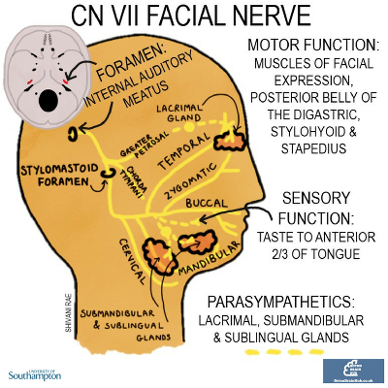
This one is a bit more complex as it is mostly motor but also has parasympathetic and special sensory functions. It emerges from the pons and passes through the internal auditory meatus.
Before exiting through the stylomastoid foramen it gives rise to two main branches:
- The greater petrosal- parasympathetic innervation to the lacrimal gland
- Chorda tympani- parasympathetic innervation to the submandibular and sublingual salivary glands and taste to the anterior 2/3 of the tongue
Once through the stylomastoid foramen, the facial nerve branches into 5 nerves which supply the muscles of facial expression.
One way to remember the names of the 5 branches is To Zanzibar By Motor Car
- Temporal
- Zygomatic
- Buccal
- Mandibular
- Cervical
This diagram shows the location of the facial nerve nucleus in relation to the fourth ventricle:
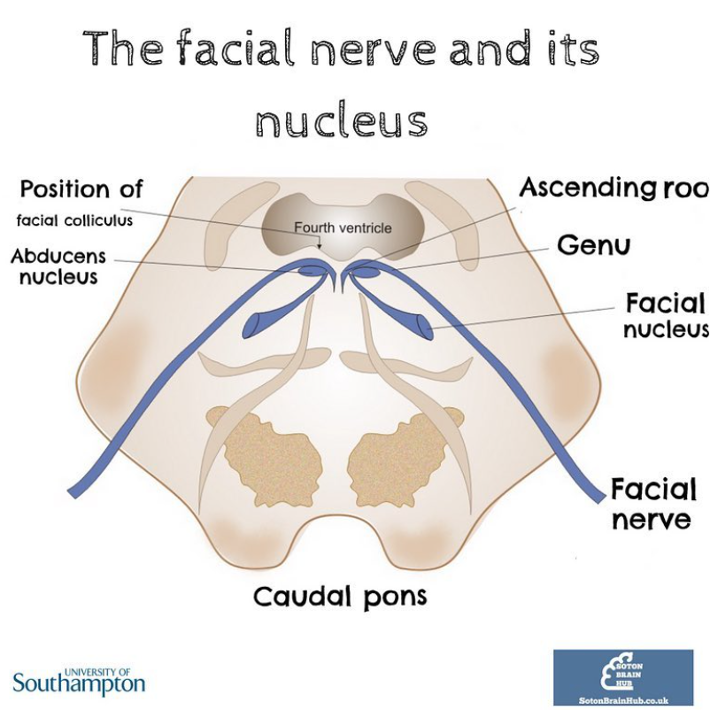
The little bump on the posterior brainstem is at the level of the caudal pons is the facial colliculus, an elevated area in the floor of the 4th ventricle. It is formed by the motor nucleus of the facial nerve as it loops around the abducens nucleus.
Check out our videos below to learn more about the facial nerve:
Clinical clue 4: Facial Nerve Palsy
Because of its long and complex course the facial nerve is susceptible to damage by infections and damage during surgery.
Damage to the facial nerve will cause paralysis of both the upper and lower half of the face on the side of the lesion.
- This can be differentiated from the facial drooping seen in a stroke by the involvement of the forehead.
Facial nerve palsy can been seen in neonates who have been delivered by forceps if there is pressure applied to the nerve
Bell's palsy is the term used for facial nerve palsy of unknown origin
CRANIAL NERVE VIII: VESTIBULOCOCHLEAR NERVE
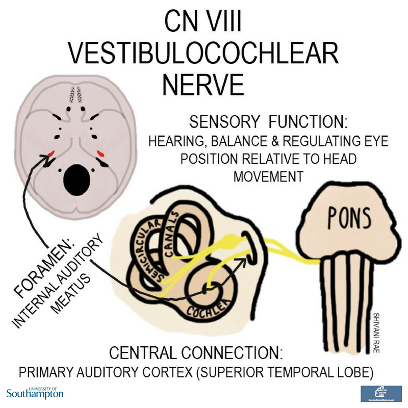
The vestibulocochlear nerve emerges from the brainstem at the cerebellopontine angle and exits the skull through the internal auditory meatus. It divides into the vestibular and cochlear nerves, both of which have sensory functions.
The vestibular nerve supplies the vestibular apparatus which includes the semicircular canals and is involved in maintaining equilibrium.
The cochlear nerve also travels to the inner ear where it mediates hearing.